Organizations often make plans for the New Year, and reflections on the past year are typically part of this process. Locke and Latham’s goal-setting theory suggests that goals should be clear and challenging, but attainable. Manufacturers want to optimize market access, and knowing what kind of access competing brands have helps to set realistic expectations for their own brands. And manufacturers may want to predict access for their new brands based on formulary analogs. But just as investors are warned that a fund’s past performance does not necessarily predict future results, payers’ past formulary decisions may not help predict their future formulary decisions.
The past
Manufacturers frequently complain about inaccurate formulary data. They know their agreements with payers and see instances when the formulary status for their brands is wrong. Most of these inaccuracies are a result of lags. First, there is the lag from when the contract takes effect to when the payer publishes the change, and this could take months. Second, there is the lag from when the payer publishes the change to when the formulary data supplier makes updates, and this could take weeks. Third, there is the lag from when formulary data are updated to when the manufacturer sees the change. A contract change, such as when a product moves from a nonpreferred to a preferred tier, may not be reflected in formulary data for several months. Formulary data may be current, but they are also history.
Before this chain of events can take place, many more months may pass before a contract can be negotiated, finalized, and take effect. By then, account managers, understandably, may be eager to see their new contract reflected in formulary data. But to maintain its status as an objective, independent third party, a formulary data supplier will want to verify this change with the payer — not simply take the manufacturer’s word. Verification takes time, and the associated lag is the basis of many perceptions that formulary data are inaccurate.
The present
Formulary data reflect payers’ policies on how drugs and biologics should be used, not how the products are actually used. The data often lack specific prior authorization (PA) criteria and step-therapy requirements. They do not suggest how liberal or conservative a payer may be with requests for formulary exceptions, redeterminations, and reconsiderations or appeals. Nor do they include information reflecting the influence of manufacturer efforts to help providers navigate PA criteria or lower patient costs through copay cards. At the end of the day, utilization or market share is where the rubber meets the road.
Patient-level prescribing data can be used to measure the impact of a formulary on utilization. In contrast to formulary data, these prescribing data are reported in near-real time. Rejection codes reveal restrictions and may suggest how manufacturers may help providers with PAs. What’s more, patient-level prescribing data can be used to infer the tier placement of products and suggest how manufacturers could adjust their patient assistance programs or contracting strategy. But supplanting formulary data with much more costly prescribing data to gain important and actionable insights requires additional analytic resources — a potentially expensive proposition. Many manufacturers may instead continue to purchase less costly formulary data despite their inherent limitations.
The recent announcement that Surescripts is partnering with six EHR companies and two PBMs to deliver patient-specific benefit and price information to providers in real time is noteworthy. This is evidence that Surescripts knows the formulary status of products and, importantly, that this information is current. Surescripts currently supports providers, PBMs, and pharmacies, but could potentially offer this business intelligence to manufacturers and challenge the two leading formulary data vendors.
The future
Formulary analogs may be used to predict future market access, but selecting the appropriate analogs is as much an art as it is a science. It should start with a nuanced understanding of the market context — not with the data. And while some market scenarios are easily described, others are not. Good luck picking the right analog for new, disruptive, and expensive technology like CAR-T therapy or gene therapy for blindness. And advanced analytics on analogs may offer little to no insights as payers approach tipping points like the shift to indication-based contracts for biologics. Formulary data may not be a leading indicator of payers’ frustration with manufacturers or their readiness to make formulary changes. Frustration, readiness to change, and associated tipping points can only be predicted through primary research. An overreliance on advanced analytics of secondary data can be deceptive, just as an overreliance on any single type of data or analytics.
Reflections
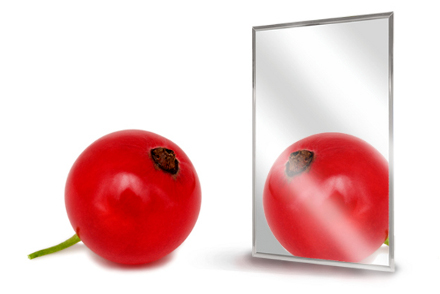
Whether the information is stale or the wrong analog is selected, formulary data have the potential to distort reality — just like a funhouse mirror or “skinny mirrors” designed to sell more clothes. To the manufacturers purchasing formulary data and/or analytics based on formulary data… buyer beware. To the sellers and analysts of formulary data, embrace the strengths and weaknesses of the data and champion a multi-method approach that triangulates qualitative and quantitative insights to get closer to the truth.


No Comments